Added Note 11th Nov: The below post may stand generally, in terms of APoB/ApoA, and HDL-C itself being linked to ApoA1 as described – but not always – apparent significant proportions of high HDL people presenting with CHD nonetheless; one possible other factor is the elevated HDL associated with excessive (detrimental) alcohol intake (credit to Irelands foremost Histopathologist Gearoid O’Laoi for recently bringing up this cunning confounder!): http://www.ncbi.nlm.nih.gov/pubmed/2862791. Also I’ve added in more recent data showing “higher HDL is a good marker for lower CAD”: http://www.thefatemperor.com/blog/2014/11/12/and-hdl-now-thats-a-tad-more-useful
So I’ll leave the post below as is, but it’s not a simple one – higher via moderate alcohol OR exercise OR weight loss OR LCHF then you good to go, but it’s not a panacea!
Original post:
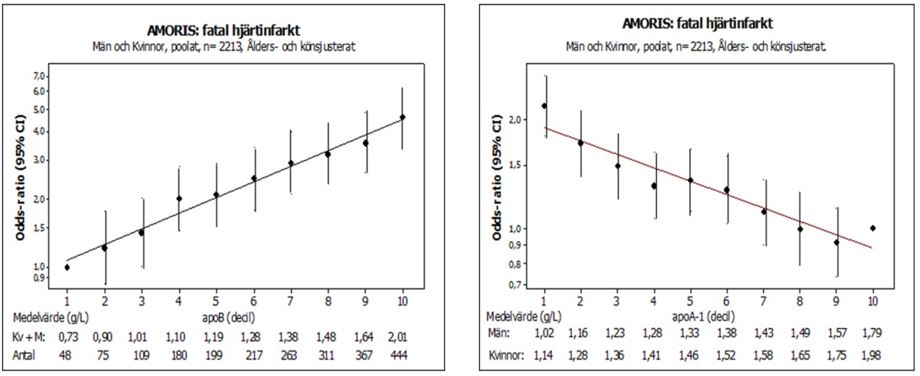
There was a little consternation recently in LCHF circles, when a piece came out suggesting HDL-C is NOT a negative risk factor for CHD etc. after all (http://ht.ly/DheeU) Huh? I was rather surprised at the assertion, as pretty much all data I have seen has been unequivocal on the matter, especially when HDL-C is included in ratio form with other parameters, and not JUST for Insulin Resistant cohort either. Mechanistic evidence agrees overwhelmingly. So how can two pillars of root cause be wrong, even in the absence of an RCT that proves finally (drug-based RCT’s for HDL have been a farce)? Let’s take a look at the lauded AMORIS Study, case-cotrol yes, but >200,000 people; we’ll see if the new assertion is mathematically probable, shall we? This study, like many others, demonstrated the primacy of ApoB/ApoA1 as THE predictor of Cardiovascular Issues. In case there’s a need for clarity, ApoB or LDL-P is the particle count, a more predictive measure than LDL-C, and Apo-AI is similarly the better proxy for HDL-C :
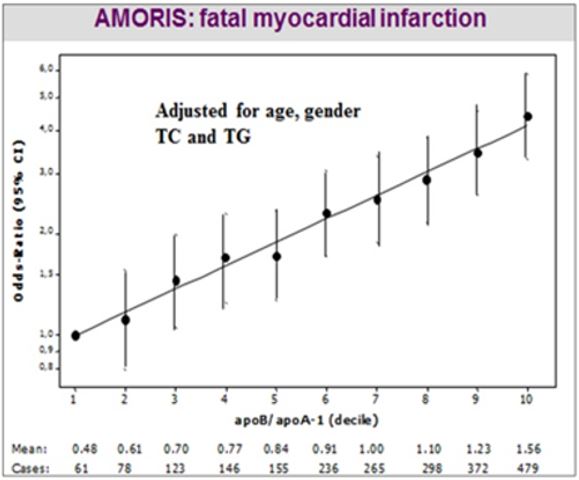
Wow – did you just see that? I didn’t make it up, although it looks too perfect to be true – but it is. And that’s a Log Scale. And the same relationship is seen in countless trials and case-control studies e.g. Interheart, one of the biggest of them all, across many countries and brutally consistent throughout. Now let’s look at ApoB and ApoA1 separated out from the same data:
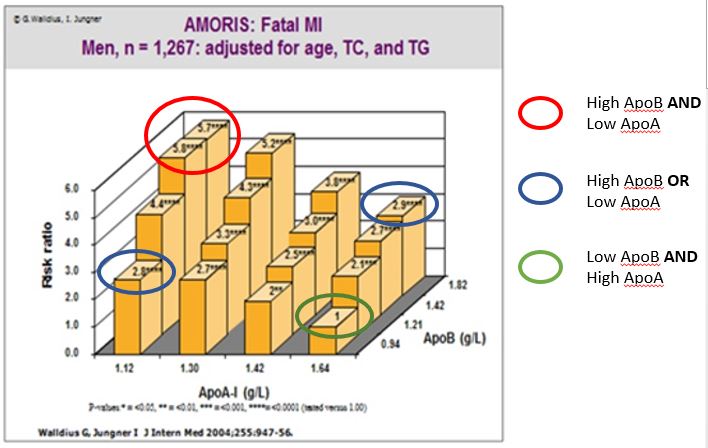
NICE! (no, not the NICE that gives medication guidelines – sometimes they’re crap). Genuine “nice”. As can be seen, high ApoB is largely equivalent to low ApoA1 in terms of risk (blue circles). Back to the assertion re: HDL: if Apo1 is not a big deal, and ApoB is the only game in town, how is low ApoA1 yielding high risk in the leftmost corner, with ApoB low? Anyway, ideally you would aim to have low ApoB and high ApoA1 simultaneously (green). And if you have high ApoB and low ApoA1 well…….don’t put off those retirement plans – do it now! Okay, we’re nearly there – because the asserters may call out: “but that’s ApoA1 – that’s not the same as HDL-C! “ Well mathematics, the highest science of all, should be given a chance to answer that – from the same dataset:
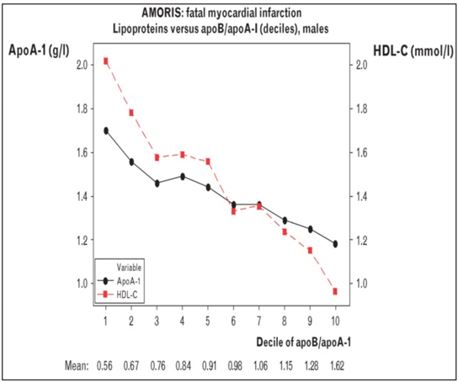
And there we have it – we can see excellent correlation between HDL-C and ApoA1. So in this excellently executed study, HDL-C will almost certainly reflect ApoA1 where it matters. And it DOES appear to matter – a lot. But do I hear someone griping “it’s not an exact proxy though?” Well the axes aren’t chosen to look at the exactness of the match – so I took the ApoA1 line and translated it quickly to check:
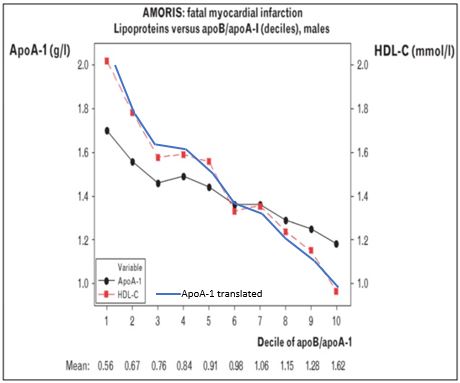
And there you have it – Red HDL-C against Blue ApoA1. Therefore:
1. ApoB/ApoA1 is THE critical predictive marker for cardiovascular risk (again and again, accepted by almost everyone in the field..)
2. Both ApoB AND ApoA1 appear to near equally contribute to the critical marker’s value.
3. HDL-C is shown as an excellent proxy for ApoA1 in REAL WORLD EMPIRICAL DATA.
4. HDL-C must be thus hugely important, as is ApoB in fairness – no questions there (except if one is LCHF and ultra-low Insulin etc)
5. HDL-C : ApoA1 and ApoB can be optimized by LCHF for the majority (and Trigs / Insulin / BG / HbA1c, Inflammation, GGT etc etc etc etc are sorted simultaneously !)
6. Sadly, chemicals can only target ApoB – that’s why I’d never take ’em – not when the obvious solution is, well, obvious.
7. There are masses of data that triangulate to the above conclusion also, but they’re not even needed to disprove the assertion.
The Fat Emperor
Nov 2014
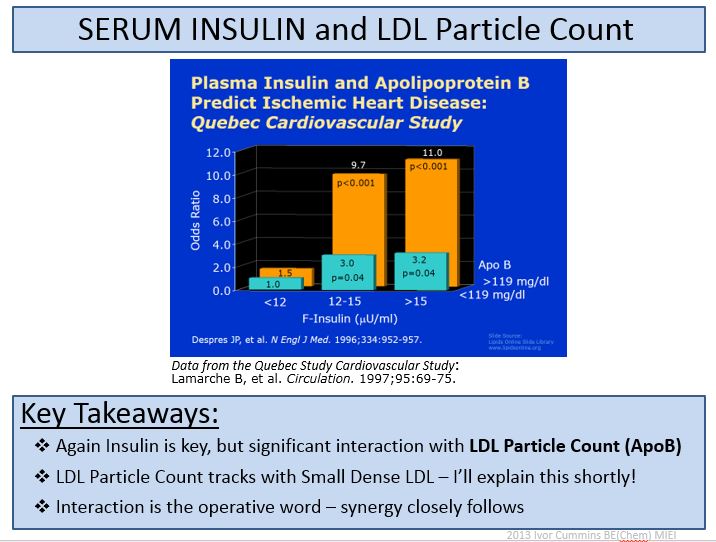
And there’s more – even if your ApoB stays genetically highish on LCHF, you’ll tend towards low Insulin, which is critical to the system. And you’ll could squirm yourself into the leftmost group from Quebec:
Yawn. A glass of wine before bed methinks. That took it out of me….
Important Reference – Swedish AMORIS Analysis
Very Important – Neovascularization Paper – Fundamental Pathology of Atheroma
Dietary Fat INCREASES HDL via Transport Rates and decreased catabolism
Apo-AI Milano reduces Thrombosis 378.full
Goran Walldius Killer APO B APO A AMORIS PAPER
Great 2009 B_A Ratios Versus Lipids for Risk