Quick post on some interesting new research sent on to me by Raymund Edwards (thanks Raymund!). Only speed-read it but good to get it out for review. The old cholesterol and atherosclerosis thing has been doing the rounds for decades, while the data points to insulin-related dysfunction being vastly more important. Here we have a team who are helping to remove the ‘cholesterol noise’ from the insulin picture. I’ll simply reproduce Raymund’s facebook post in full below. Bottom line is that they’ve produced a mouse model which separates the ‘cholesterol confusion’ from the ‘insulin resistance imperative’. They have in short demonstrated atherosclerotic acceleration through insulin-mediated action – WITHOUT the cholesterol confounding. Cholesterol metrics gone awry are most often a by-product of insulin/glucose dysfunction, and the ‘cholesterol’ gets mistaken for cause. So kudos to these researchers – if we had work like this a few decades ago, we might not be suffering the diabetic farce that we are in today…
Don’t forget to subscribe for more of the relevant data at www.thefatemperor.com/subscribe
The paper: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3891225/ and Raymund’s summary excerpts below:
“Some background to this group headed by Sonia M. Najjar
They have a NUMBER of studies planned
–> Individuals with metabolic diseases are at a higher risk of developing atherosclerosis, a leading cause of death in the United States and worldwide.
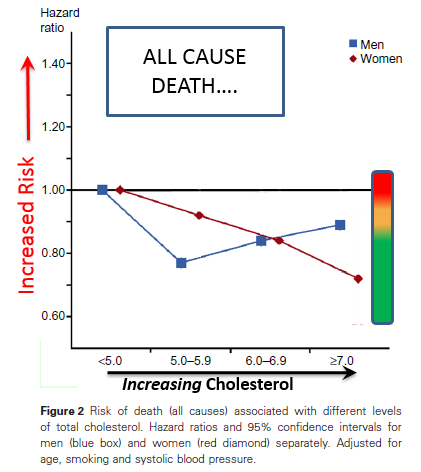
Earlier studies have linked dyslipidemia to the initiation and progression of atherosclerosis. However, recent clinical studies raised concerns about the efficacy of lowering plasma cholesterol levels in the progression of atherosclerosis. Although insulin resistance is associated with increased incidence of cardiovascular disease, whether it leads to atherosclerosis independently of its accompanying dyslipidemia remains unclear, largely because of the lack of a suitable animal model to address this question.
The CarcinoEmbryonic Antigen-related Cell Adhesion Molecule-1 (CEACAM1) regulates insulin sensitivity by promoting insulin clearance in liver. Accordingly, global null deletion of Ceacam1 gene impairs hepatic insulin clearance and causes hyperinsulinemia, which in turn, results in systemic insulin resistance.
Preliminary data show: (i) that global Cc1–/– null mice develop early atherosclerotic lesions and vascular dysfunction even under normal feeding conditions, and (ii) that this occurs in the absence of hyperlipidemia, despite VLDL/LDL cholesterol levels that are usually associated with atherosclerosis regression, not development.
This unique animal model of atherogenesis with isolated insulin resistance in the absence of hyperlipidemia demonstrates that systemic insulin resistance resulting from hyperinsulinemia leads to vascular dysfunction and atherosclerosis in the absence of hyperlipidemia.
Because phosphorylation of CEACAM1 by both insulin and VEGF receptors regulates Akt1 activation of endothelial Nitric Oxide Synthase (eNOS), an essential step in mediating endothelial function, it is reasonable to propose that CEACAM1 is the shared downstream element in VEGF and insulin signaling in endothelial cells, whose inactivation impinges upon both pathways and causes endothelial dysfunction in insulin resistance.
==> The CarcinoEmbryonic Antigen-related Cell Adhesion Molecule-1 (CEACAM1) is a membrane with ubiquitous expression in many cell types, including liver and endothelial cells, but not skeletal muscle and adipose tissue. CEACAM1 regulates insulin sensitivity by promoting insulin clearance in liver.
We and others, have shown that mice with global deletion of Ceacam1 gene (Cc1–/–) exhibit hyperinsulinemia, resulting from impaired hepatic insulin clearance. Hyperinsulinemia in these mice leads to insulin resistance, increased liver triglyceride content and de novo lipogenesis, which drive VLDL-ApoB secretion and triglyceride accumulation in adipose tissue, causing visceral obesity and raising serum fatty acid levels. Thus, the Cc1–/– mouse is a
model of hyperinsulinemia causing insulin resistance.
•• Preliminary data show: (i) that Cc1–/– mice with global Ceacam1 deletion spontaneously develop early atherosclerotic lesions with impaired endothelial-dependent vasodilation under normal feeding conditions, and (ii) that this occurs despite VLDL/LDL cholesterol levels that are usually associated with atherosclerosis regression, not initiation.
Therefore, Ceacam1 deficiency causes hyperinsulinemia and insulin resistance, and promotes lipid-independent vascular toxicity. This makes Cc1–/– a unique animal model of spontaneous
atherosclerosis with isolated insulin resistance in the absence of hyperlipidemia, and provides an in vivo demonstration of distinct CEACAM1-dependent mechanisms linking insulin resistance to atherosclerosis.
• Ceacam1 deletion causes vascular alterations in large vessels