UPDATE 7th July: The learned Peter Dobromylskyj of Hyperlipid has posted on this fascinating subject – ignore the cholesterol goons and get some education here 🙂 http://high-fat-nutrition.blogspot.ie/2016/07/arteriosclerosis-6-and-subbotin.html
What constitutes a valid, actionable ‘Root Cause’? I have my definition, been good for over 25 years of problem-solving:
“When an Issue manifests itself, Root Cause is the interplay between (A) The most direct modifiable driver of the issue (usually situated early in the root cause chain diagram), and (B) the most addressable factor to achieve acceptable solution (usually it will be the factor/input that has actually shifted and driven the problem itself”
There may be multiple coincident factors that are implicated as worthy of Root Cause status by the way – especially in the nasty multi-factor issues. And Atherosclerosis is certainly one of those. Of course interaction and synergy is extremely important to decode – some ’causes’ are only relevant when other real/driving ones are present – gotta tackle the latter.
I am happy with the dominant probable root causes of Atherosclerosis. These are excessive carbohydrate/sugar (Inflammatory/IR/multiple), low Sun/VitD (Inflammatory/IR/multiple), Low Omega3:6 ratio (Inflammatory/IR/multiple – esp. filthy veg oils), low Magnesium(multiple), bad sleep/stress (glycaemic/insulin/IR), low K2/C and a few other vitamins (multiple). Insulin Resistance is a no-brainer, hence the ‘IR’ thrown regularly in there. But I’m still more interested in what key factors gave you the IR of course(!). The pareto principle is useful here – focus on the 20% of factors that likely cause 80% of your issues. Why didn’t I mention Gut Microbiome? Well until proven otherwise, I think it is often a outcome of the preceding RC list, which then in turn causes knock-on issues by all means. Why didn’t I mention ApoB particles in the list? Well because they wouldn’t meet my definition of root cause, would they? ApoB particles are physiologic – they are normal to have, almost regardless of their quantity. Of course if they were damaged … or elevated due to a real ‘root cause’ (read IR etc.), then they get warmer. But even here they would be too far down the root cause chain for my liking – they would also be ‘knock-on’ drivers…
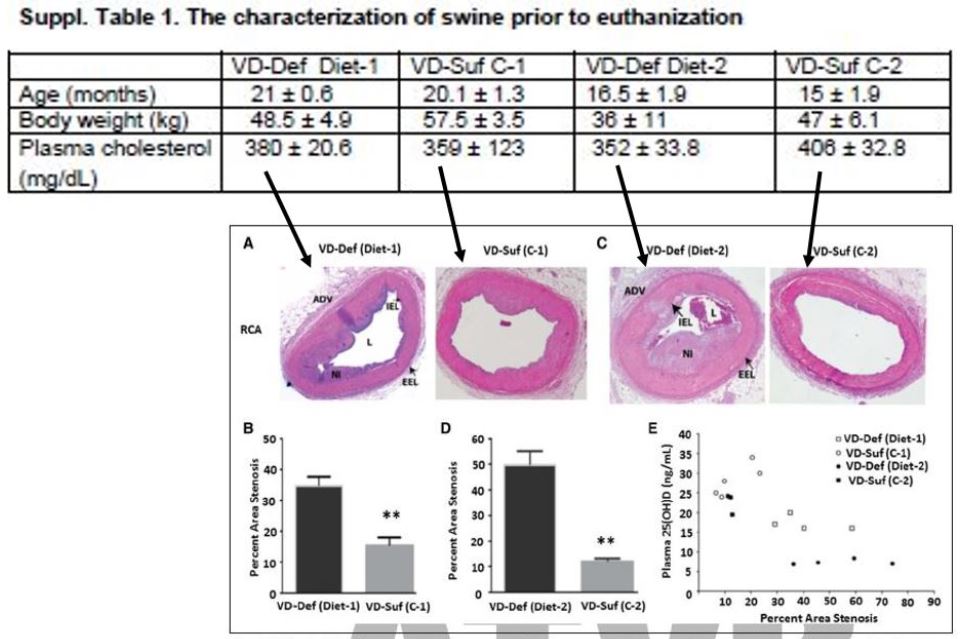
So, what have we got for you today? Well thanks to George Henderson, a rather fascinating atherosclerosis experiment just published – that’s what. (http://atvb.ahajournals.org/content/early/2016/06/02/ATVBAHA.116.307586.abstract ). And the effect-size seen was, well – impressive to say the least. These guys were not caught up in ApoB – they were switching on and off a real root cause – and it seems to have paid off. They gave very little Vitamin D to some pigs, and adequate amounts to others. They fed them all a horror-show junkfood diet to accelerate atherosclerosis, then killed them all after a year or so. (Diet of course had high sugar and chocolate etc. – they know what blows up IR & atherosclerotic fires). What did they see? Well get a load of this:
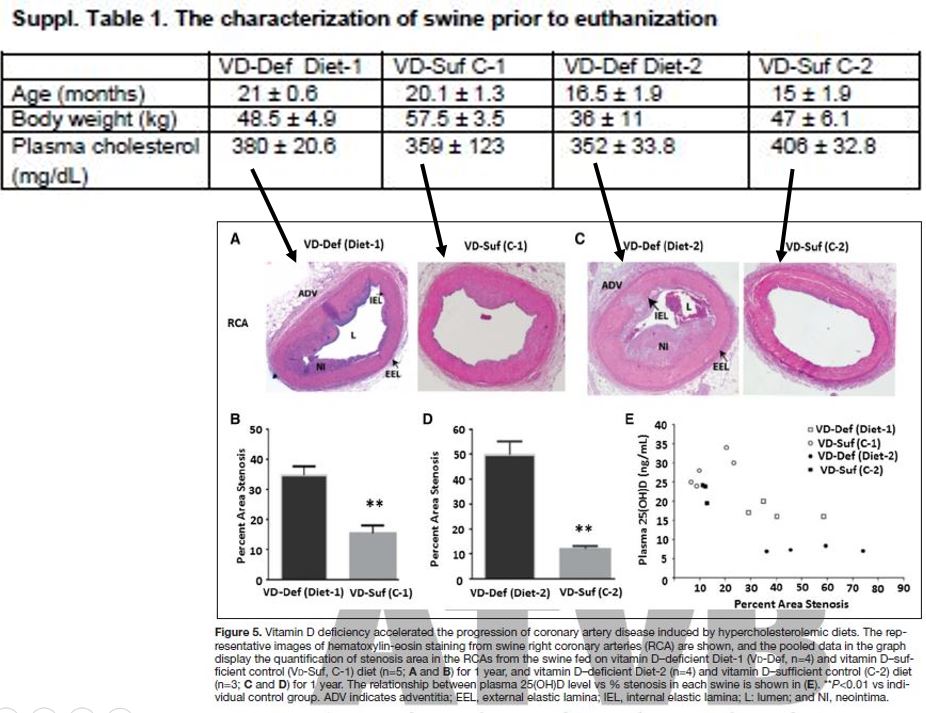
Note that ‘cholesterol’ again shows itself up as the correlational junk science that it is. But let’s look at an excerpt of their conclusions (my emphasis included). This is VERY interesting:
“Studies have shown that the administration of inflammatory mediators outside the arterial adventitia leads to immune cell invasion, increases in intimal thickness, and arterial remodeling (40,41) and increased coronary vasa vasorum neovascularization PRECEDES endothelial dysfunction in swine fed a high-cholesterol diet (42,43). These data suggest that local adipokines from EAT could diffuse into interstitial fluid across the adventitia into the vascular wall by paracrine factors or be directly transported into downstream coronary arteries by vasocrine factors (i.e. via the vasa vasorum). This hypothesis supports a notion of outside to inside signaling of atherosclerosis, in which the inflammatory milieu in EAT promotes the development and progression of CAD. Recently, in atherosclerotic swine, McKenney et al11 clearly showed that EAT excision attenuated the progression of CAD, but their observation did not have a clear mechanistic link. Here, we provide critical data on EAT signaling mechanisms underlying CAD.”
Interesting indeedy. Time is brief here so I’ll give my top-level takeaways:
1. Vitamin D deficiency seems to has a dramatic effect on Atherosclerosis progression, like a ‘root cause’ should if it is valid (I have some quibbles that their diets do not seem to be identical outside of the D factor though)
2. They clearly provide support for Subbotin’s hypothesis of vasa vasorum being pivotal in atherosclerosis progression – and add other ‘outside-in’ mechanisms of acceleration from the external surface of the arteries (i.e. NOT the endothelial-ingress concentration gradient stuff that many of us have struggled with)
3. They leave ApoB out of the discussion – fair enough. It’s not a ‘root cause’ that can be changed in magnitude to assess its contribution. In it’s native (non-damaged) self It’s not really a ’cause’ as such by my definition – even though it has mechs in the athero game, and it is supported by much ‘correlational’ data (although much of this correlation was likely gifted by the insulin resistance which drives both it and athero acceleration up together – sneaky stuff – see: http://www.thefatemperor.com/blog/2015/5/5/hilarious-apob-now-being-used-as-predictor-of-insulin-resistance-cholesterol-lchf).
I’ll also direct interested parties to this post, for further ruminations on ApoB as a ’cause’. Real ’causes’ stand up to case-control and other scrutiny – but correlational ones don’t:
…and of course an overview of Subbotin’s atherosclerosis mechanisms paper – I am still waiting for anyone to give a reason or two why Subbotin may be incorrect. After this pig study, the reasons would want to be pretty solid indeed…
For more always-free content please subscribe at www.thefatemperor.com/subscribe